Revitalizing Rural Care: Sutter Health’s Bold Move to Expand Behavioral Health Access | PRIMENEWSNOW

Addressing Behavioral Health Gaps in Rural Areas
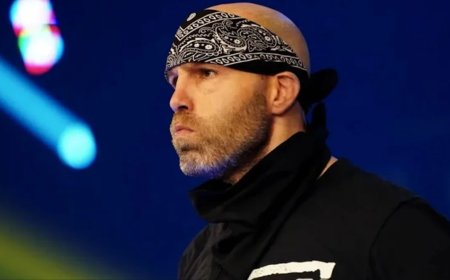
Rural communities face significant challenges in accessing behavioral health services. In honor of National Rural Health Day on November 20, Sutter Health’s Dan Peterson, CEO of Behavioral Health Services, and Dr. Matthew White, chair of the Behavioral Health Service Line, discuss their efforts to enhance access to these services in Northern California’s rural regions. They highlight the role of crisis stabilization units, investments in rural clinics, and virtual psychiatry in supporting both patients and healthcare providers in these underserved areas.
Expanding Behavioral Health Access
Behavioral health resources are scarce in many rural parts of the country. Sutter Health is committed to significantly increasing access to these services for rural residents in Northern California. Their strategy extends beyond merely building new facilities, as discussed by Dan Peterson and Dr. Matthew White.
Understanding Sutter Health’s Reach
Sutter Health is a comprehensive healthcare system focused on Northern California, operating 23 hospitals and employing 57,000 staff, including 6,000 physicians. Their facilities range from urban centers like San Francisco to small towns near the Oregon border, supporting numerous rural hospitals and clinics.
Critical Access Hospitals: A Lifeline
Critical access hospitals serve as the sole healthcare providers in rural areas, meeting specific geographic criteria. Dan Peterson shares his experience as CEO of Sutter Lakeside Hospital, emphasizing the vital role these hospitals play in communities where residents often cannot travel long distances for care.
Investments in Rural Health Infrastructure
Sutter Health is making significant investments in rural areas, such as constructing new office buildings for primary and urgent care in Crescent City and developing an empath unit for behavioral health crises. Additionally, a new rural health clinic is set to open in Los Banos, integrating behavioral health services into primary care.
Innovative Crisis Care Solutions
Dr. Matthew White explains the empath unit, a specialized crisis stabilization facility designed to provide a calming environment for those in behavioral crises. This approach has been shown to reduce hospitalization rates and lengths of stay, offering a more therapeutic alternative to traditional emergency rooms.
Community Collaboration and Support
Community partnerships have been crucial in developing these initiatives. Sutter Health has worked closely with local organizations and tribal entities to secure funding and support for projects like the empath unit, demonstrating the power of collaboration in rural settings.
Leveraging Virtual Psychiatry
To address the shortage of psychiatrists in rural areas, Sutter Health is utilizing tele-psychiatry and collaborative care models. These approaches allow primary care physicians to access psychiatric support, enhancing patient care and maximizing the available workforce.
Benefits of Integrated Care
Integrated care models not only improve patient satisfaction but also enhance workforce morale and reduce stigma, particularly in rural communities. By supporting clinicians to practice at the top of their license, Sutter Health is effectively meeting the needs of rural patients.
Conclusion
Dan Peterson and Dr. Matthew White’s efforts to improve behavioral health access in rural areas highlight the importance of innovative solutions and community collaboration. As National Rural Health Day approaches, these initiatives serve as a reminder of the ongoing need to support rural healthcare systems.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0